What is Spinal Cord Stimulation (SCS) Therapy?
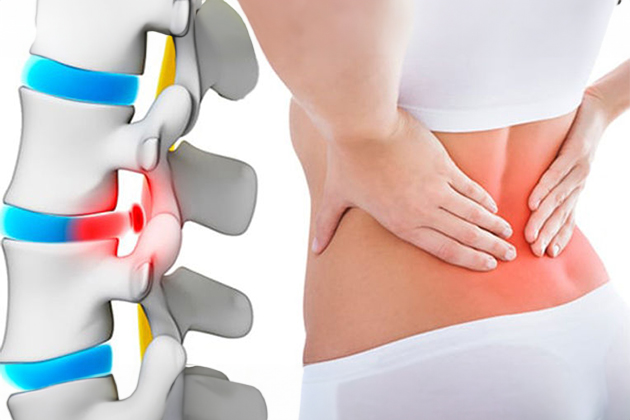
Spinal Cord Stimulation (SCS) therapy is a treatment method used for managing chronic pain. This therapy employs a system of electrodes placed near the spinal cord. These electrodes send electrical signals that block or alter pain signals, thereby reducing the level of pain felt by patients. SCS is commonly used for conditions such as back pain, leg pain, or neuropathic pain. Although the therapy does not completely eliminate pain, it can significantly improve the quality of life for many patients.
When is Spinal Cord Stimulation (SCS) Therapy Commonly Used?
- Chronic Back and Leg Pain: Particularly in cases of failed back surgery syndrome.
- Complex Regional Pain Syndrome (CRPS): Characterized by intense and persistent pain.
- Peripheral Neuropathy: Pain resulting from nerve damage.
- Ischemic Pain: Conditions such as peripheral vascular diseases or angina pectoris.
- Radiculopathy: Pain due to nerve root damage.
SCS is typically considered when other treatment methods (medication, physical therapy, surgery) have not been sufficient or have not yielded the desired results. This therapy offers an alternative method for pain management and aims to enhance the patients’ quality of life.
The Surgical Decision-Making Process in Spinal Cord Stimulation (SCS) Therapy
- Assessment of Pain and Medical History: The patient’s history of chronic pain, previous treatments, and overall health are thoroughly evaluated.
- Trial of Other Treatments: Medication, physical therapy, injections, or other non-surgical treatments are tried. If these do not provide adequate results, SCS is considered.
- Psychological Evaluation: The patient’s psychological state and expectations from SCS therapy are assessed. Conditions like depression or anxiety may influence the treatment process.
- Trial Period: A short-term trial with a temporary electrode system is conducted before the permanent SCS device is implanted. During this trial period, the patient’s pain level and response to treatment are observed.
- Evaluation of Success Criteria: If pain is reduced by at least 50% during the trial period, a decision is made to implant the permanent device.
- Surgical Decision: If all evaluations are positive, a decision is made to implant the permanent SCS device, and surgical planning is done.
Outcomes of Spinal Cord Stimulation (SCS) Therapy
The outcomes of SCS therapy can vary based on the patient’s general condition, the severity of pain, and individual response to treatment. Generally:
- Reduction in Pain: Most patients report a 50% or greater reduction in pain, significantly improving their quality of life.
- Reduced Medication Use: Decreased pain can lead to reduced use of pain medications, especially opioids, avoiding their side effects.
- Improved Functional Capacity: Patients may find it easier to perform daily activities and may experience increased general physical activity.
- Improvement in Psychological State: Reduced pain can lead to lower levels of depression, anxiety, and stress, positively affecting overall mental health.
- Side Effects and Complications: While SCS carries some risks, such as infection, device failure, or displacement, these are generally manageable.
- Long-Term Effects: Some patients report sustained effectiveness of SCS over the long term, while others may experience a decrease in effectiveness over time. Regular device checks and adjustments can enhance long-term success.
Risks and Possible Complications of Spinal Cord Stimulation (SCS) Therapy
- Infection: Infection may develop around the device implantation site or around the electrodes placed near the spinal cord, sometimes requiring antibiotic treatment or device removal.
- Device Failures: Malfunctions in the SCS device or electrodes may occur, necessitating readjustment or replacement.
- Electrode Displacement: Electrodes may shift, reducing stimulation effectiveness or causing unwanted sensations, necessitating repositioning.
- Surgical Complications: Risks include bleeding, wound healing problems, or complications related to anesthesia.
- Allergic Reactions: Allergic reactions to the device components or materials used during surgery can occur.
- Nerve Damage: Though rare, nerve damage during surgery can lead to temporary or permanent neurological symptoms.
- Skin Erosion: Skin erosion around the device or electrodes may necessitate device removal.
- Unwanted Stimulation Sensations: Patients may find the stimulation sensations uncomfortable or experience them in unexpected areas.
- Economic and Psychological Burden: The cost of the device and ongoing maintenance may be financially burdensome, and some patients may experience stress or anxiety related to the treatment or device implantation.
Living with a Spinal Cord Stimulator
Living with a spinal cord stimulator can significantly enhance the quality of life for many people with chronic pain, but it requires some adjustments and careful attention:
- Pain Reduction: Most patients experience significant pain reduction due to the electrical signals from the stimulator, enabling easier performance of daily activities.
- Regular Check-Ups: Regular medical check-ups are necessary to ensure the stimulator functions correctly, during which device settings are optimized.
- Device Maintenance and Usage: Attention to the battery life and charging status of the stimulator is crucial. Some stimulators are rechargeable, while others require periodic battery replacement.
- Physical Activity: Patients should avoid heavy lifting, high-impact sports, or other activities that might displace the device.
- Electromagnetic Fields: Strong magnetic fields, metal detectors, or certain medical devices may interfere with the stimulator’s function, so these should be avoided.
- Situations Requiring Device Deactivation: The stimulator may need to be turned off during flights or certain medical procedures (e.g., MRI scans), following doctor’s instructions.
- Psychological and Emotional State: Improvement in pain management can positively affect psychological and emotional well-being. However, adjusting to the stimulator’s presence may take time and some patients may initially struggle to adapt.
- Side Effects and Complications: Management of potential side effects or complications, such as infection or device malfunction, should be done in consultation with a healthcare professional.
- Quality of Life: Overall, patients using SCS report significant improvements in pain management, mobility, and the ability to perform daily activities, leading to an enhanced quality of life.
Featured Videos
Frequently Asked Questions
Craniotomy is a surgical procedure used in the treatment of brain tumors, involving the opening of the skull. Neurosurgeons use this fundamental method to access and remove tumors.
Physical Activity: Gradually return to physical activities following your neurosurgeon’s recommendations. This typically starts slowly and increases over time. Physical activity can improve muscle strength and endurance, but it is important not to overdo it.
Rest: Adequate rest is crucial during the recovery period. Sleep aids in brain healing. Paying attention to your sleep schedule will be beneficial.
Balanced Diet: A healthy and balanced diet supports your recovery process. Follow the recommendations of your neurosurgeon or a dietitian to ensure you receive the necessary nutrients.
Regular Use of Medications: If you have postoperative medications, take them regularly as directed by your doctor.
Cognitive Exercises: Brain tumor surgeries can sometimes affect cognitive functions. Mental exercises can support memory, thinking, and concentration skills. Solving puzzles, reading books, or playing mental games can be beneficial.
Doctor Check-Ups and Follow-Up: Regularly visit your doctor and follow your neurosurgeon’s recommendations to monitor and manage your postoperative process.
Psychological Support: Emotional and psychological challenges can occur after brain tumor surgeries. Psychologists or support groups can help.
Support Systems: Family, friends, and community support are critical during the recovery process. It’s important to seek help when needed.
Returning to Work or School: When you wish to return to work or school, do so slowly with your doctor’s approval. You may request a flexible work or school schedule.
Infections: The surgical incision or area can become infected, leading to wound infections or more serious infections like meningitis.
Brain Swelling (Edema): Swelling in the brain may occur post-surgery, causing headaches, nausea, vomiting, and neurological symptoms. It is usually treated with corticosteroid medications.
Bleeding: Bleeding can occur during or after surgery, potentially requiring surgical intervention.
Cognitive Issues: Brain tumor surgeries can sometimes lead to memory loss, concentration problems, speech difficulties, or other cognitive issues. These are often temporary but can sometimes be permanent.
Neurological Problems: Temporary neurological issues may occur post-surgery, including weakness, numbness in limbs, or balance problems.
Vulnerability and Blood Clots: Post-surgery patients are at risk of blood clots due to inactivity. Measures should be taken against deep vein thrombosis (DVT) or pulmonary embolism.
Medication Side Effects: Postoperative medications can cause side effects. Corticosteroids or anticonvulsants, in particular, may lead to certain side effects.
Urinary Issues: Problems related to urination, such as bladder control or urinary tract infections, can occur after brain tumor surgeries.
Drug Tolerance: Some patients may respond differently to medications post-surgery, affecting pain management and other treatment options.
Psychological Effects: Psychological impacts such as anxiety, depression, or emotional changes can occur after brain tumor surgeries.
Each patient is different, and potential risks vary depending on the type of tumor, the extent of surgery, and the patient’s overall health condition.