What Situations are Most Commonly the Cause?
In our daily lives, a significant portion of spinal traumas is caused by injuries following traffic accidents and falls from heights. Spinal fractures and injuries can occur in any part of the spine, from the neck to the tailbone. Spinal injuries often occur at the junction of the most mobile parts of the spine, between the thoracic and lumbar vertebrae (between the 12th thoracic vertebra and the 1st lumbar vertebra, T12 – L1). Seventy percent of fractures occur in the thoracic and lumbar vertebrae, 5-10% in the cervical vertebrae, and the remainder in lower regions.
What are the Symptoms?
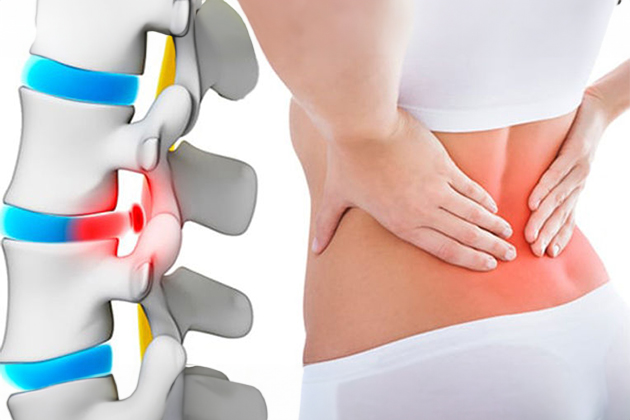
Depending on the location of the lesion, patients may experience neck, back, or lower back pain. Typically, there is sudden onset neck, back, or lower back pain following trauma. The pain worsens with standing or walking. Spinal fractures due to osteoporosis can also develop without a history of trauma. Since the pain in fractures resulting from osteoporosis can be tolerable, the patient may continue their daily life without noticing the condition. A compression fracture of the spine can lead to further height loss in the bone over time, distorting the spine and the patient’s posture, resulting in a condition known as kyphosis (hunchback).
If a spinal fracture has caused damage to the spinal cord or the nerves emerging from it, various forms of paralysis can be seen in patients. The patient may be unable to move their arms or legs, and this weakness may be accompanied by a loss of sensation. Bladder and bowel control may also be impaired.
How is Diagnosis Made?
The patient’s medical history, complaints, and examination findings are very important for diagnosis. An X-ray (direct radiograph) is the first test to be performed on patients suspected of having an injury. Often, it can successfully show the alignment of the spinal bones and any collapses or displacements in them. A computed tomography (CT) scan provides detailed information about the structure of the spinal bones. It clearly shows broken bone fragments that have entered the spinal canal. It provides information about the amount, shape, and type of the fracture. Magnetic resonance imaging (MRI) provides more information about the soft tissues in the spine. Thus, detailed information about the spinal cord, nerve tissue, cartilage, ligaments, and connective tissue is provided. As a result, spinal cord damage, traumatic hernias accompanying spinal fractures, bleeding around the spinal cord, and tears in ligaments and connective tissue can be thoroughly evaluated.
How is Treatment Carried Out?
Conservative (Protective) Treatment
Conservative protective treatment is often sufficient. The main goal here is to reduce the movement of the traumatized spine to both accelerate healing and reduce pain. Bed rest for varying durations, depending on the shape and location of the fracture, along with the use of a brace, can be applied. Painkillers, movement restriction, brace usage, and medications to increase bone strength and density can enable the bone to heal itself. Surgical treatment is considered when medical treatment is insufficient.
What is Surgical Treatment? When is it Necessary?
Surgery is required in patients whose pain cannot be controlled or whose spinal collapse is at critical levels. The primary goal is to relieve the spinal cord and nerve roots that are under pressure.
Minimally Invasive Surgery
In this method, under local anesthesia and special imaging techniques, thick needles are used to reach the fracture area. Depending on the condition of the fracture, the collapsed part can be raised with cement (kyphoplasty) or filled directly (vertebroplasty). This eliminates the pain in the collapsed spine and strengthens it. Patients can be sent home the same day or the next day after these procedures.
Spinal Fusion Surgery
In some cases, patients are not suitable for this treatment. In such cases, open surgery is performed. Open surgery involves removing bone fragments that are pressing on the spinal cord. The fractured vertebral bodies are replaced with metal cages or supportive bone structures. To ensure proper alignment and restore load-bearing capacity, the vertebrae may need to be stabilized with titanium screws and rod systems. Grafts taken from the body or prepared externally can be used to support and enhance bone fusion.
Frequently Asked Questions
Symptoms of a vertebral compression fracture include sudden onset or progressively worsening back or waist pain, loss of height, kyphosis (hunchback), limited mobility, and numbness, tingling, or weakness in the legs due to pressure on nerve roots.
A vertebral compression fracture is diagnosed through physical examination and imaging tests. X-rays show the height of the vertebrae and the location of the fracture. MRI provides more detailed information about nerve roots and soft tissues. CT scans also allow for a detailed examination of the fracture. Additionally, a bone density test (DEXA) is used to assess the presence of osteoporosis.
To prevent a vertebral compression fracture, it is important to maintain and strengthen bone health. Adequate intake of calcium and vitamin D, regular exercise, avoiding smoking and excessive alcohol consumption, maintaining a healthy diet, and taking necessary precautions to reduce osteoporosis risk factors are essential. Regular bone density checks can also ensure early diagnosis and treatment of osteoporosis.
Treatment options include non-surgical methods and surgical interventions. Non-surgical treatments involve rest, pain relievers, physical therapy, the use of braces, and osteoporosis treatment. Surgical treatments include vertebroplasty, kyphoplasty, and spinal fusion. The choice of treatment method depends on the severity of the fracture and the patient’s overall health condition.