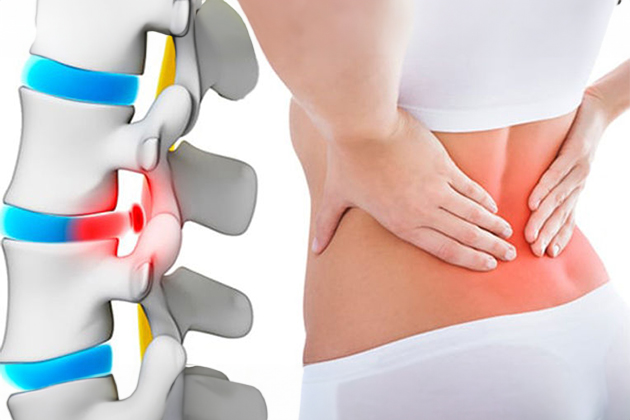
Can a Herniated Disc Recur?
Yes, a herniated disc can recur.
What Does Recurrence of a Herniated Disc Mean?
Recurrence of a herniated disc means that the disc, which had previously been herniated and treated surgically, herniates again after a certain period. Both lumbar and cervical disc surgeries carry a risk of recurrence. The risk is higher in lumbar disc cases compared to cervical disc cases. Studies indicate that 10-20% of patients who undergo lumbar disc surgery experience recurrence. In some studies, this risk is reported to be as high as 25%. These risk percentages can vary depending on the patient’s specific condition, lifestyle, and the success of the surgery.
Factors That Increase the Risk of Recurrence:
- Age: As age increases, the spinal tissue may wear out, increasing the risk of degeneration and recurrence of the hernia.
- Overloading: Lifting heavy objects, sudden high-impact activities, and poor body mechanics (lifting heavy loads in incorrect positions) can damage the spine and increase the risk of hernia.
- Smoking: Smoking can negatively affect circulation and tissue healing capacity, increasing the risk of hernia recurrence.
- Obesity: Carrying excess weight can put additional stress on the spine and increase the risk of hernia.
- Genetic Predisposition: A family history of spinal issues may increase the likelihood of hernia due to certain genetic factors.
- Physical Activity Level: Low physical activity levels can lead to the weakening of muscles and connective tissues, reducing spinal support and increasing the risk of hernia.
- Poor Posture: Poor posture can cause abnormal loading of the spine, increasing the risk of hernia.
- Trauma or Injury: Previous spinal injuries or traumas can affect spinal stability and increase the risk of hernia.
- Occupational or Activity-Related Risks: Certain professions or activities that consistently lead to spinal injuries may increase the risk of hernia.
- Chronic Pain: Chronic back or neck pain can create continuous pressure and stress in the spinal area, increasing the risk of hernia.
Measures to Prevent Recurrence of a Herniated Disc:
- Physical Activity: Regular, low-impact exercises can reduce the risk of hernia recurrence. Exercises that strengthen the back and abdominal muscles can improve spinal stability. Activities like swimming, walking, and yoga can aid spinal health.
- Weight Control: Maintaining a healthy weight can reduce the additional pressure on the spine and lower the risk of hernia recurrence.
- Good Posture: Maintaining good posture is crucial for spinal health. Proper sitting, standing, and lifting techniques can help maintain correct spinal alignment.
- Proper Lifting Techniques: Using correct body mechanics when lifting heavy loads is very important. Creating a wide base of support with your feet and bending your knees while lifting can prevent excessive spinal pressure.
- Warm-Up and Cool Down Before Exercise: Performing warm-up exercises before physical activity and cool-down exercises afterward can prepare the muscles and spine and reduce the risk of injury.
- Ergonomic Work Environment: Ensuring that the work desk and chair are ergonomic can help maintain spinal health, especially if working in an office. Keeping the computer screen at eye level is important.
- Stress Management: Stress can increase muscle tension and put extra pressure on the spine. Stress management techniques can help relax muscles.
- Avoid Smoking and Excessive Alcohol Consumption: Smoking and excessive alcohol consumption can negatively affect spinal health. Avoiding these harmful habits can reduce spinal problems.
- Regular Check-Ups: Individuals with a history of hernia should have regular doctor check-ups before symptoms reappear.
- Appropriate Treatment and Physical Therapy: When hernia symptoms recur, getting appropriate treatment is important. Physical therapy can reduce pain, strengthen muscles, and improve spinal health.
Treatment of Recurrent Herniated Disc:
Treating recurrent herniated discs can be more complex and treatment options may vary based on the severity of symptoms, the patient’s overall health, the location of the hernia, and other factors.
Conservative Treatment:
- The first step is usually conservative treatment, which may include rest, pain relievers, anti-inflammatory medications, physical therapy exercises, hot or cold applications, and spinal traction. This approach can be effective for mild or moderate symptoms.
Medications:
- Prescription medications can be used to manage pain and inflammation, including pain relievers, muscle relaxants, and corticosteroids.
Physical Therapy:
- Physical therapy programs aim to strengthen muscles and improve spinal stability, potentially alleviating hernia symptoms and reducing the risk of future recurrence.
Injections:
- Intrathecal steroid injections or epidural steroid injections can help reduce inflammation and alleviate pain. These injections can provide temporary relief for some patients.
Spinal Traction:
- Spinal traction aims to reduce pressure on the spinal discs and relieve hernia symptoms.
Surgical Intervention:
- If recurrent hernia symptoms are severe and unresponsive to treatment or cause neurological problems, surgical intervention may be necessary. Surgical options include microdiscectomy or endoscopic discectomy (removal of herniated discs) and laminectomy (partial removal of spinal bones). Surgery aims to remove the disc material compressing the nerve roots and alleviate pressure. Sometimes, hernias are accompanied by spinal slippage. In such cases, removing the bone structure behind the spine to relieve the spinal cord and performing a fusion surgery (fusing the vertebrae together using metal instruments) may be necessary.
Frequently Asked Questions
A herniated disc occurs when the outer layer of the discs in the spine tears and the gel-like substance inside comes out, pressing on the nerve roots. This condition can happen due to heavy lifting, sudden movements, or aging.
Symptoms of a herniated disc include lower back pain, pain that radiates from the hip to the leg (sciatica), numbness or tingling in the legs, weakness in the legs, and limited mobility. The pain may increase with coughing or sneezing.
A herniated disc is diagnosed based on the patient’s complaints and physical examination findings. Imaging methods such as MRI, CT, and X-ray are used to confirm the diagnosis and determine the location of the herniation.
The recovery process varies depending on the type of surgical intervention performed and the patient’s overall health condition. Postoperative physical therapy and rehabilitation are important to speed up recovery and maintain spinal health. Patients should adhere to the exercise program recommended by their doctor, use prescribed medications for pain management, and avoid heavy lifting or strenuous activities.