Structure and Function of the Spine
Our spine is composed of interconnected bone structures called vertebrae. Our lower back consists of five vertebrae and cushioning pads between them called discs. The spine transfers the load from our torso to the hips and legs and supports our posture. It helps us stand upright while allowing for bending movements in all directions. The vertebrae are connected by disc cushions and joints called facet joints. Additionally, the supportive ligaments and muscle tissue around the vertebrae keep them tightly connected. These structures bear the body’s load, helping us maintain an upright position while allowing specific movements.
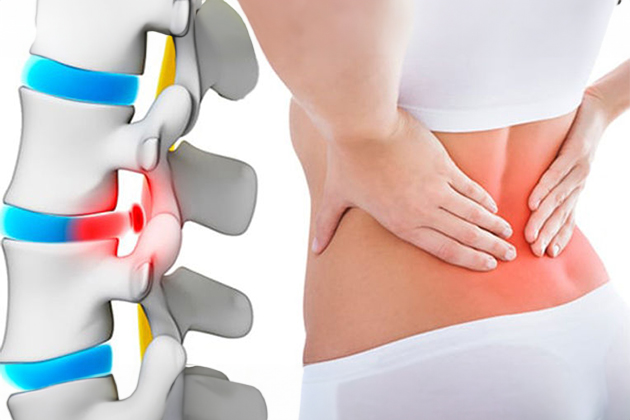
Structure of Discs and Lumbar Hernia
Discs are strong connective tissues that link the vertebrae and act as cushions. They consist of a robust outer layer called the annulus fibrosus and a gel-like center called the nucleus pulposus. As we age, the nucleus pulposus loses water content, failing to function as a cushion. This situation leads to the nucleus pulposus moving through a tear in the outer layer, creating a condition called a lumbar hernia. Lumbar hernias typically occur in the last two discs located in the lower back and just below the lower back. A herniated disc can cause back pain and pressure on the nerves exiting the spine, leading to pain, numbness, and weakness in the legs, a condition known as sciatica.
Lumbar Hernia Treatment Options
Short-term Rest and Medication:
- Pain relievers to control pain
- Physical therapy
- Exercises
- Epidural injections
Avoiding Long-term Rest:
- Prolonged bed rest can cause stiffness in the joints and weakness in the muscles, making it challenging to perform pain-reducing movements.
- Mild stretching exercises and posture changes are recommended.
Physical Examination and Diagnosis:
- Straight leg raise test indicating sciatic pain
- Muscle weakness, numbness, reflex changes
- Imaging methods like MRI and CT scans to definitively identify nerve compression.
Microdiscectomy:
- Most commonly used methods:
- Microsurgical discectomy using a microscope (Microdiscectomy)
- Endoscopic discectomy using an endoscope
Surgical Process:
- Performed under spinal or general anesthesia.
- The patient lies face down on the operating table.
- A small incision is made on the skin over the herniated disc space, and the muscles over the spine are stripped from the bone.
- A small piece of bone may be removed to see the compressed nerve.
- The herniated disc and broken pieces are removed to relieve nerve compression.
Post-surgery:
- An incision smaller than 2 cm is made.
- The patient is made to walk 6 hours after the surgery and is discharged after staying in the hospital for one night.
Post-surgery Care:
- Avoid driving for the first four weeks.
- Avoid prolonged sitting, heavy lifting, and bending forward.
- Move your body part in line with your hips and shoulders.
- Start with slow movements and increase your activity level.
- Avoid lifting heavy objects.
- You can participate in physical therapy or a rehabilitation program.
- Pay attention to your sleep and rest pattern.
- Ensure a balanced diet.
- Avoid smoking and alcohol.
- Avoid stress, practice meditation, or deep breathing exercises.
- Continue regular doctor check-ups.
Non-surgical Treatments
Radiofrequency Thermocoagulation:
- Damaged nerve tissue is destroyed using radiofrequency energy.
Transforaminal Injection:
- Steroid or anesthetic agents are injected into the nerve roots.
Facet Joint Injection:
- Steroid or anesthetic agents are injected to relieve pain in the facet joints.
Ozone Therapy:
- Damaged tissue is oxygenated using ozone gas, reducing inflammation.
These treatment methods are used to alleviate the symptoms of lumbar hernia and improve patients’ quality of life. Your neurosurgeon will evaluate the patient’s condition to determine the appropriate treatment method.
Featured Videos
Frequently Asked Questions
The diagnosis of a herniated disc is based on the patient’s complaints and physical examination findings. Imaging methods such as MRI (Magnetic Resonance Imaging), CT (Computed Tomography), and X-ray can be used to confirm the diagnosis. Additionally, an EMG (Electromyography) test can be used to determine the degree of nerve damage.
The symptoms of a herniated disc include lower back pain, pain radiating from the hip to the leg (sciatica), numbness or tingling in the legs, leg weakness, limited mobility, and rarely, incontinence. Pain may increase with coughing, sneezing, or prolonged sitting. The fundamental pathology of a cervical herniated disc arises from the compression or tearing of the cervical spine discs. This condition prevents the discs from performing their normal functions and exerts pressure on the surrounding nerve tissues. The leakage of the gel inside the discs can cause inflammation and nerve damage. Therefore, the mechanism of cervical herniated disc disease includes both mechanical and inflammatory components.
Surgical treatment is preferred in the following situations:
If pain does not subside with medical treatment
If the severity of pain is increasing
If you are unable to perform daily life activities
If there are serious issues like significant muscle weakness and incontinence
Surgical treatment is generally recommended to relieve the patient from leg pain and to prevent progressive muscle weakness. This treatment has a success rate of over 90%.
The recovery process after herniated disc surgery varies depending on the type of surgical intervention and the patient’s overall health condition. Postoperative physical therapy and rehabilitation are important to accelerate the recovery process and maintain spinal health. Post-surgery considerations include adhering to the exercise program recommended by the doctor, using prescribed medications for pain management, and avoiding heavy lifting or strenuous activities. Regular check-ups and compliance with the doctor’s instructions are also crucial during the recovery process.
